Inflammation is increasingly recognized as a significant risk factor for heart disease, diabetes, and certain cancers. Much like a car running hot signals an impending breakdown, chronic inflammation in the human body can lead to serious health problems. This article explores the link between inflammation and various diseases and offers expert advice on how to manage and reduce chronic inflammation…Click Here To Continue Reading>> …Click Here To Continue Reading>>
The Dual Nature of Inflammation
Inflammation is a crucial component of the body’s defence mechanism. It mobilizes the immune system to fight off bacteria and other pathogens, or to repair damage such as that from a sprained muscle. Infections often trigger a raised temperature, and injured areas can become warmer than the surrounding healthy tissue. However, when this short-term response fails to deactivate properly, or unhealthy lifestyle choices keep it simmering in the background, prolonged inflammation can significantly increase the risk of cardiovascular disease, type-2 diabetes, arthritis, cancer, and many other chronic conditions.
The Impact of Chronic Inflammation
Studies estimate that three out of five people will die from diseases linked to chronic inflammation. Another study found that 50% of all deaths are due to conditions associated with inflammation, including heart disease, stroke, cancer, diabetes, chronic kidney disease, non-alcoholic fatty liver disease, and autoimmune and neurodegenerative conditions.
Professor Claire Bryant from the Department of Medicine at Cambridge University is a leading expert on inflammation. She explains that the NLRP3 inflammasome, a particular protein complex, plays a crucial role in many major diseases, including obesity, atherosclerosis, Alzheimer’s, and Parkinson’s disease. “Inflammation seems to underpin most diseases of old age. As we age, we enter a condition called inflammaging, where we have higher markers for inflammation in the blood,” she notes.
This age-related inflammation is linked to the reduction in muscle mass, bone strength, and immunity, all of which are hallmarks of ageing.
Warning Signs and Risk Factors
Identifying chronic inflammation can be challenging, as there are no reliable tests. Routine blood tests often include checks for C-reactive protein, a marker for inflammation, but these are designed to measure short-term flare-ups associated with infections or injuries, rather than chronic inflammation. Symptoms of chronic inflammation are often dismissed as the results of busy lifestyles or ageing and can include aches and pains, insomnia, chronic fatigue, depression and mood disorders, gastric symptoms like constipation, diarrhoea, acid reflux, weight gain or loss, and frequent infections.
Several risk factors for chronic inflammation have been identified, including ageing, obesity, diets high in refined sugar and saturated and trans-fats, smoking, stress, sleep disorders, and low levels of sex hormones such as estrogen and testosterone. These risk factors often interact, creating a vicious cycle. For instance, a diet high in sugar and fat can lead to weight gain, poor sleep increases the risk of obesity, and hormone levels decline with age.
Professor Bryant highlights the cyclical nature of inflammation: “Inflammation can start to ramp up and get out of control because once it starts, it becomes a vicious cycle. It requires intervention with medication and lifestyle changes.”
Medical Measures and Treatments
Research has shown that medications used to treat heart disease and diabetes also reduce inflammation. Statins, commonly prescribed for lowering cholesterol, also reduce inflammation, which helps protect against hardening of the arteries and coronary heart disease. Similarly, metformin, a diabetes treatment, has been found to dampen chronic inflammation. Scientists are still investigating the mechanisms behind this anti-inflammatory effect, but a study suggested that metformin could be repurposed to address a range of complications, including inflammation, infections, and even cancer. READ FULL STORY HERE>>>CLICK HERE TO CONTINUE READING>>>
Fasting and Inflammation
Studies have shown that fasting can reduce inflammation. Both alternate-day fasting and time-restricted eating, where daily calorie intake is confined to a narrow window, have been proven to lower inflammation, provided they lead to a reduction in body weight of at least 6%. Professor Bryant’s research revealed an unexpected mechanism behind this reduction: fasting increases levels of arachidonic acid, an omega-6 fatty acid previously identified as a driver of inflammation. “There could be a yin and yang effect, where too much of the wrong thing increases inflammasome activity and too little decreases it,” she explains. However, she advises against fasting without consulting a doctor, especially for individuals with conditions like diabetes.
The Role of Fats in Inflammation
The types of fats we consume can influence inflammation levels. Saturated fats are particularly harmful because they increase the odds of being overweight and short-circuit the immune system, driving inflammation. Maintaining a balance between omega-6 and omega-3 fatty acids is also crucial. Historically, the ratio of omega-6 to omega-3 in our diet was around 4:1, but the typical Western diet now has a ratio closer to 20:1, which may promote low-level inflammation.
Omega-3 fatty acids, found in oily fish, have well-documented anti-inflammatory properties. Professor Philip Calder from the University of Southampton has shown that omega-3 fats DHA and EPA give rise to resolvins, which are anti-inflammatory and help resolve inflammation.
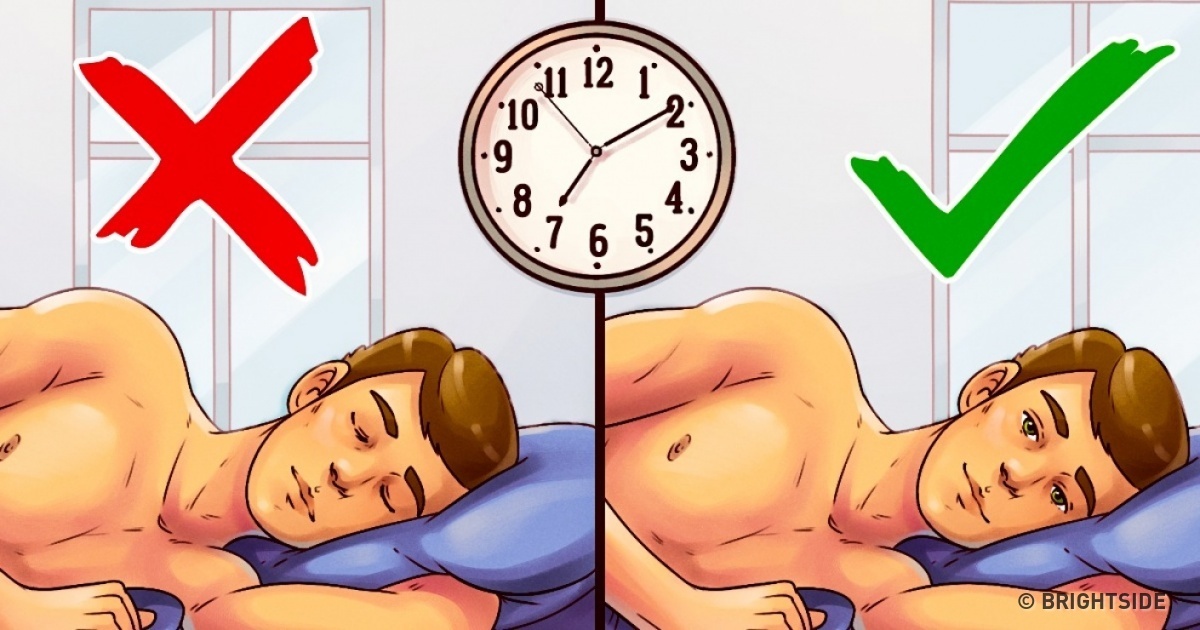
The Importance of Sleep
Disrupted sleep increases the risk of various health problems associated with inflammation. Researchers at Oxford University found that good sleep patterns can reduce the risk of dying from cardiometabolic diseases by up to 39% and from cancer by up to 19%. Inflammation appears to be a key driver of this link. Poor sleep also increases the risk of obesity and cravings for high-fat, high-sugar foods, perpetuating the cycle of inflammation.
Exercise and Inflammation
Exercise is a proven method to combat inflammation and many age-related diseases. Short bursts of intense activity are particularly effective, but even 20 minutes of exercise a day can lower inflammation. Resistance training is also beneficial and aligns with NHS advice to engage in at least 150 minutes of moderate activity per week.
In conclusion, chronic inflammation is a hidden driver of many serious health conditions, but it can be managed through a combination of medication, diet, lifestyle changes, and exercise. By understanding and addressing the factors that contribute to inflammation, we can reduce our risk of heart disease, diabetes, cancer, and other chronic illnesses.


 METRO9 months ago
METRO9 months ago
 SPORTS10 months ago
SPORTS10 months ago
 IN-THE-NEWS5 months ago
IN-THE-NEWS5 months ago
 METRO10 months ago
METRO10 months ago
 SPORTS9 months ago
SPORTS9 months ago
 IN-THE-NEWS10 months ago
IN-THE-NEWS10 months ago
 IN-THE-NEWS5 months ago
IN-THE-NEWS5 months ago
 IN-THE-NEWS10 months ago
IN-THE-NEWS10 months ago